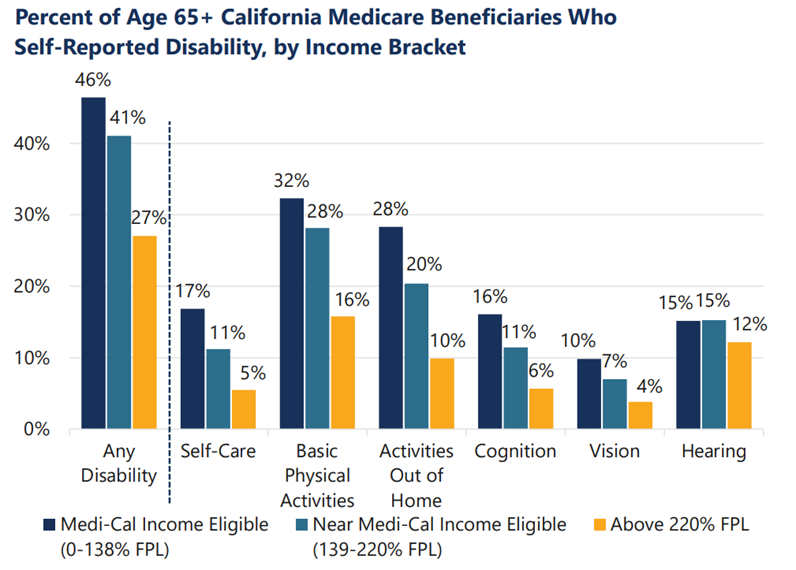
For decades, states have been working to integrate care to improve access to high-quality care for people dually eligible for Medicare and Medicaid, but progress is limited. Multisector Plans for Aging (MPAs) can support a process by which states can navigate the infrastructure and political constraints that have historically prevented states from advancing Medicare-Medicaid integration efforts.
In a new Health Affairs blog, TSF explores how an MPA can help states navigate barriers to advancing integrated, high-quality health care.