Ten Questions to Better Understand and Serve Your Complex Care Population
summary
This policy brief highlights 10 questions health plans and systems nationwide could consider using in their risk assessments to deliver more cost-effective, quality care.
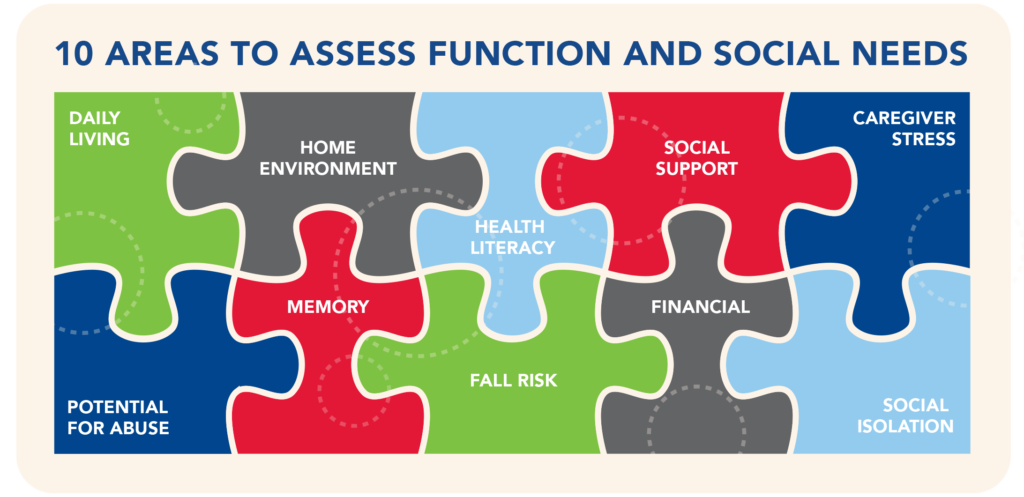
Date Updated: 04/02/2018The CHRONIC Care Act and new CMS guidance promote assessment of functional and social needs as part of delivering more cost-effective, quality care to individuals with complex needs. This brief shares 10 questions required of California’s Medicaid managed care plans, which health plans and systems nationwide could consider for their risk assessment instruments.
Overview
Health systems often identify individuals as “high cost,” “high need,” and/or “high risk” by using administrative and clinical data captured as part of medical billing. These data include items such as diagnoses, emergency department utilization, and prescription drug costs. While this easily accessible, medically oriented information provides an initial snapshot of care complexity, research shows that non-medical factors – how a person functions on a daily basis and the extent of one’s social supports – significantly affect overall health care utilization and spending.1 In fact, it costs twice as much to care for older adults with chronic conditions and functional limitations compared to those with chronic conditions alone (Figure 1).2,3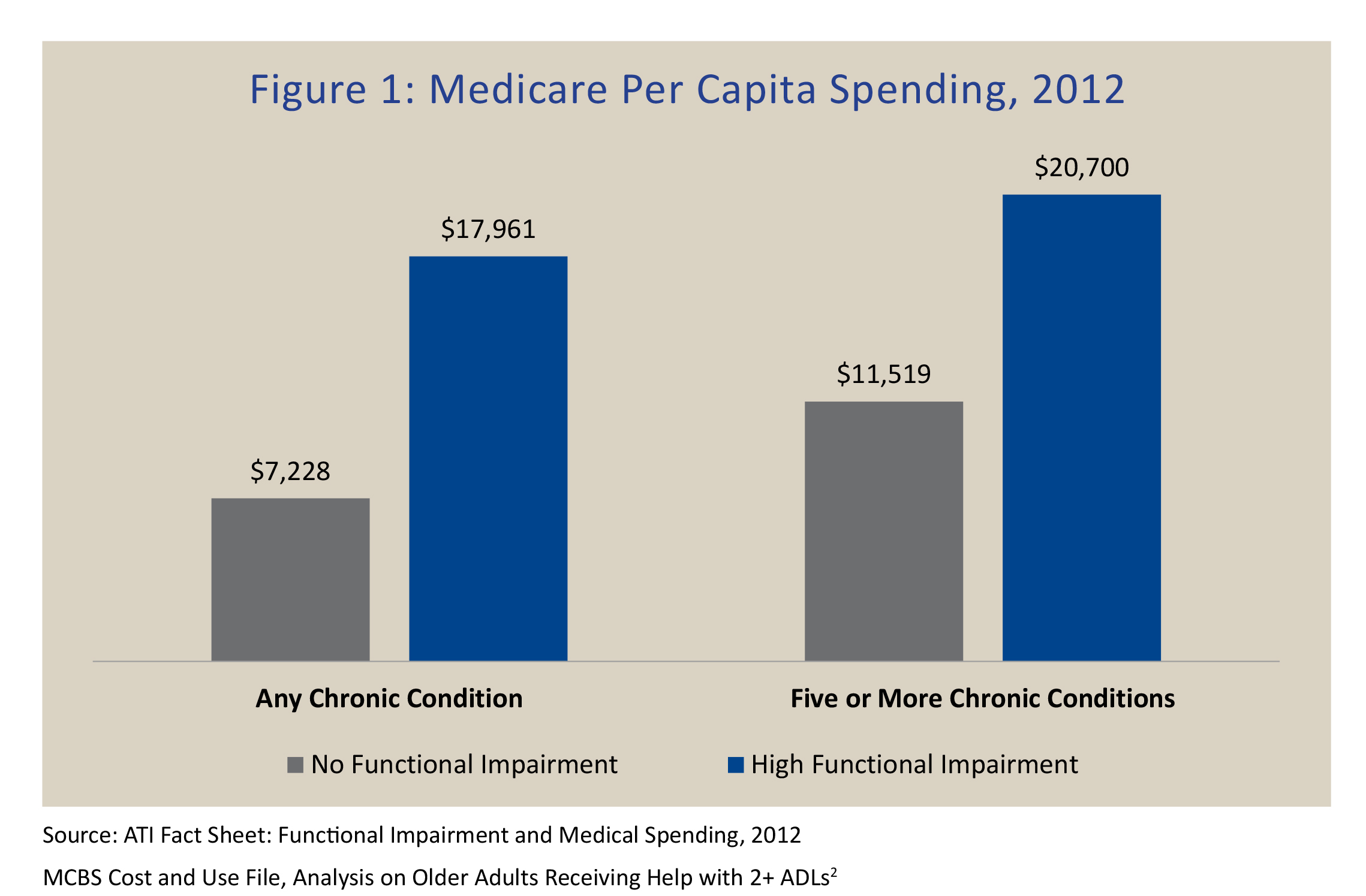
To better understand the populations they serve and effectively organize care, leading health plans and accountable care organizations (ACOs) are beginning to gather person-level data about social determinants of health (i.e., access to food, housing). The risk assessment is a natural process point for health plans and ACOs to include questions that specifically capture an individual’s functional and social support needs. This new knowledge can provide a clearer understanding of a person’s total need profile, and how it affects their health status; improve population-level risk stratification; and support delivery system efforts that better match people who have identified needs with high-quality, targeted interventions.1
Federal policymakers are fueling this trend by promoting more comprehensive assessments and linking those with complex care needs to appropriate services inside and outside of health care.
Recent policy actions include the following:
- In a draft Medicare Advantage and Part D 2019 Call Letter, federal officials recognized that health risk assessment (HRA) tools must assess beneficiaries for medical, functional, cognitive, psychosocial, and mental health needs. Medicare Advantage plans will be allowed to offer beneficiary incentives for HRA completion beginning in 2019.4
- The Call Letter and the CHRONIC Care Act also expanded the scope of supplemental benefits in Medicare Advantage that beneficiaries could receive based on a comprehensive needs assessment.4,5
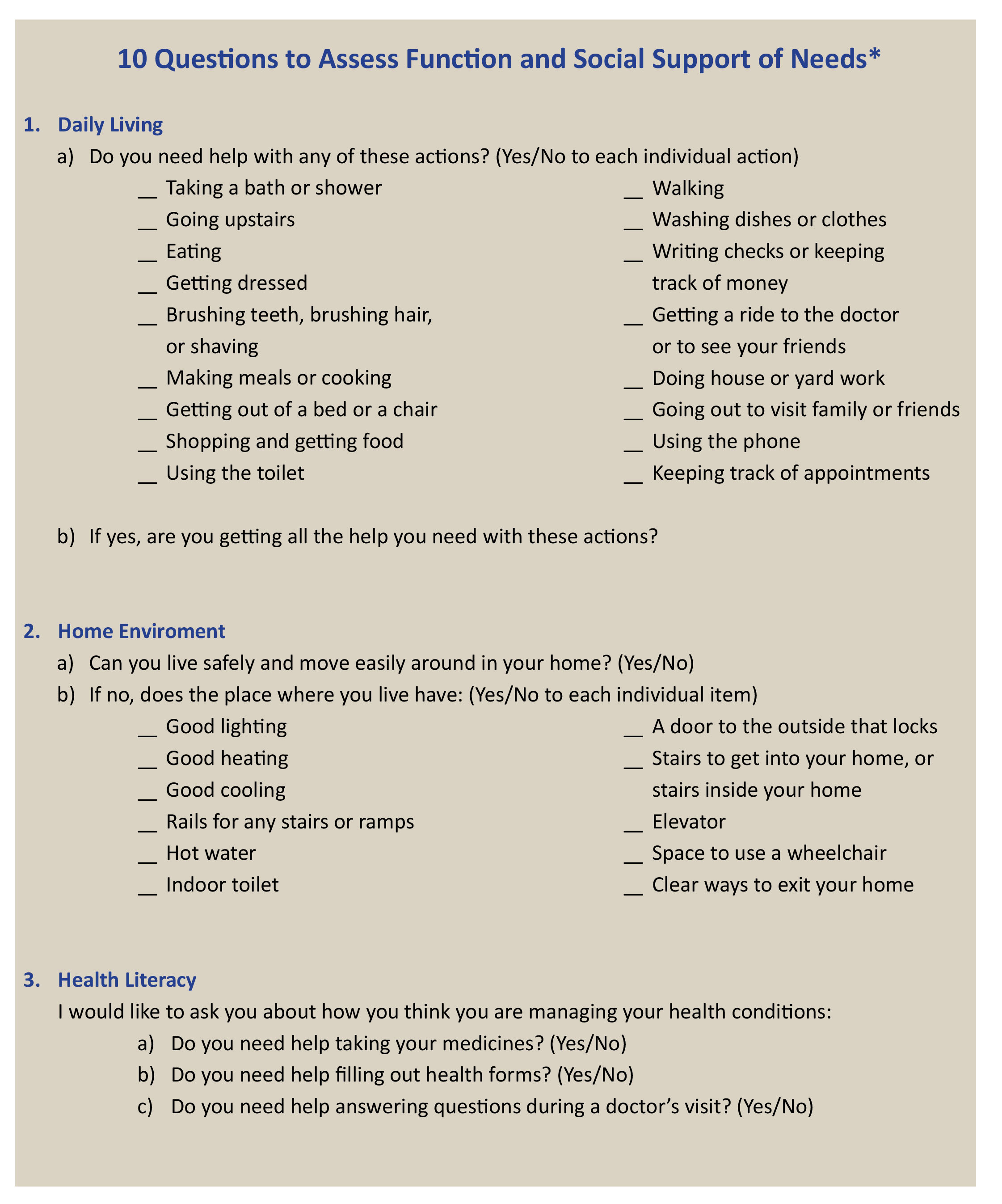
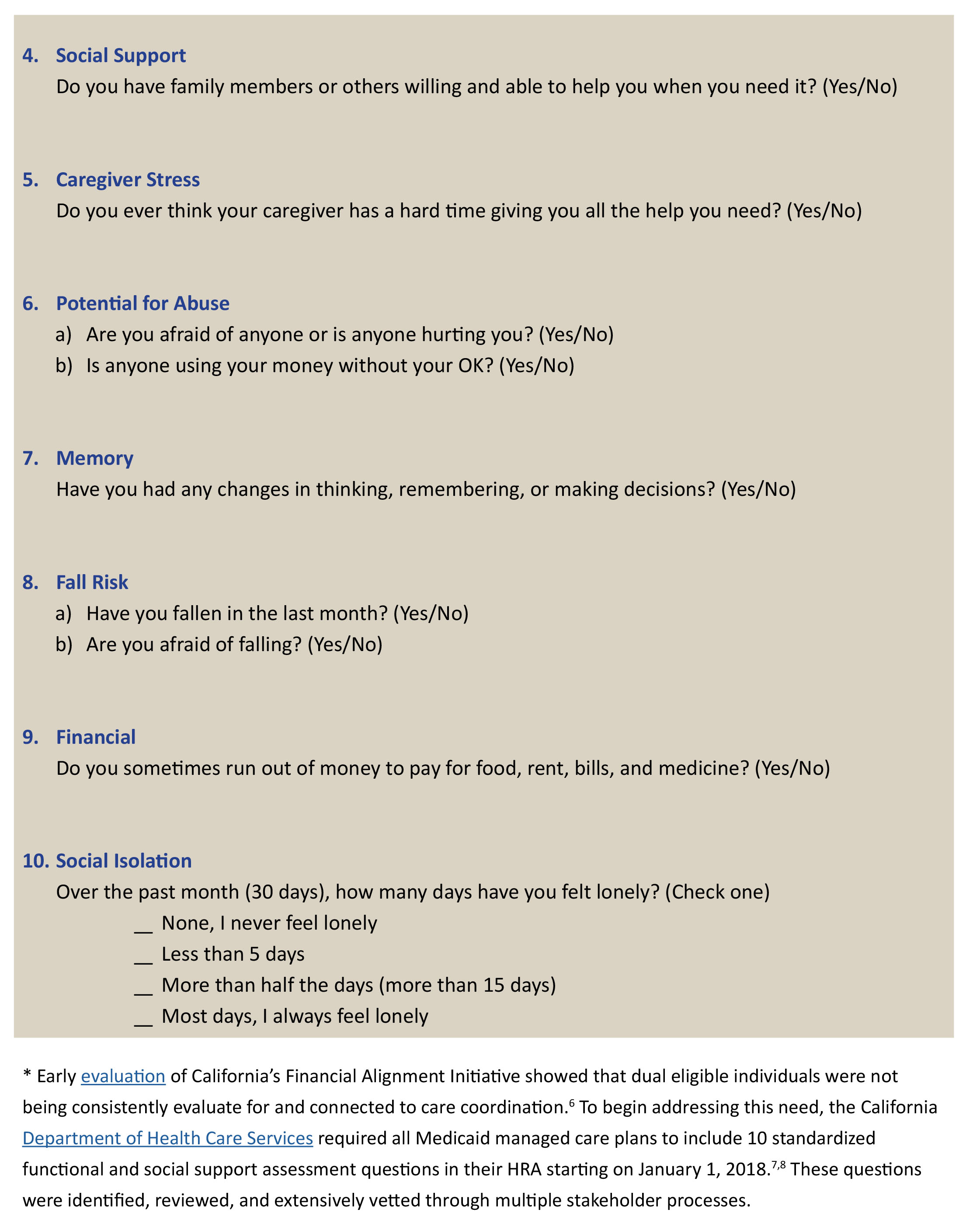
California has taken a major step in this regard, as the state recently required all Medicaid managed care programs to incorporate 10 questions in their HRA that evaluate for function and social support needs. As leaders in health plans, ACOs, and other risk-bearing entities revisit their assessment tools for better management of complex care populations, below are the 10 questions to consider for inclusion.
Download the publication for all visuals and complete references.
Continue Reading
This policy brief provides an introduction to The SCAN Foundation’s CLASS Technical Assistance Brief Series, which explores many of the critical issues to be considered for successfully implementing CLASS.
This policy brief describes the broad needs of individuals with disability and the wide range of supportive and environmental solutions that can allow for the most independent living possible. It suggests how findings on social and environmental supports for individuals with disability can inform implementation of CLASS.
This policy brief provides background on the historical development of benefit eligibility triggers in the private long-term care insurance market. Understanding how these triggers came into being can provide important information to those charged with implementing the CLASS Plan.