What Matters Most: Essential Attributes of a High-Quality System of Care for Adults with Complex Care Needs
summary
This primer document describes the Essential Attributes of this system and the core elements detailing how delivery systems should function to meet the goal, and key definitions of concepts. Collectively, they represent the milestones that, when regularly monitored and measured, can track progress toward the goal.
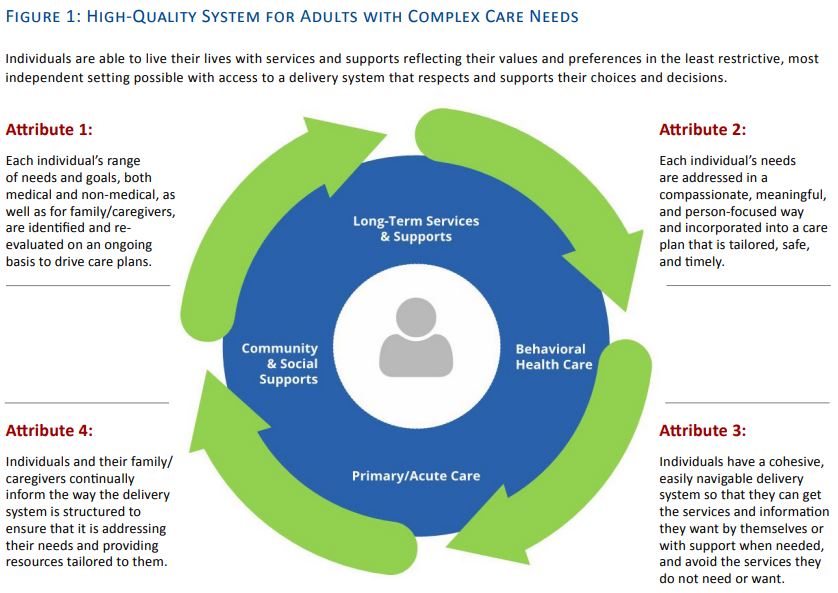
Date Updated: 08/15/2016The SCAN Foundation, with the support of the Alliance for Health Reform and Health Management Associates, convened a working group comprised of a diverse array of national experts working on behalf of adults with complex needs within the fields of health, long-term services and supports (LTSS), quality measurement, and consumer advocacy. Through a consensus process, this working group developed a goal statement and four Essential Attributes of a high-quality system of care that supports system transformation and evaluation, and is from the vantage point of adults with complex care needs (Figure 1).
The group concluded that the overarching goal of a high-quality system of care for adults with complex care needs is: individuals are able to live their lives with services and supports reflecting their values and preferences in the least restrictive, most independent setting possible with access to a delivery system that respects and supports their choices and decisions.
This document describes the Essential Attributes of this system, their core elements detailing how delivery systems should function to meet the goal, and key definitions of concepts in Figure 1. Collectively, they represent the milestones which, when regularly monitored and measured, can track progress toward the goal. The working group acknowledged that resources and sustainability
are key issues, but were not the focus of this effort.1 Figure 1 depicts the connected continuum of the Essential Attributes around the individual and the care and supports they receive.
Essential Attributes
The national working group identified four Essential Attributes of a high-quality delivery system serving and supporting adults with complex care needs. These Essential Attributes are intended to help guide future efforts to transform delivery systems and develop quality measures that capture individuals’ goals, preferences, and desired outcomes.
ATTRIBUTE 1: Each individual’s range of needs and goals, both medical and non-medical, as well as for family/caregivers, are identified and re-evaluated on an ongoing basis to drive care plans.
Delivery systems:
- Appropriately and adequately identify adults with complex care needs;
- Assess each individual’s needs in a comprehensive and holistic way, to the extent desired by the individual;
- Identify each individual’s goals, preferences, strengths, and values by a care team member with whom the individual and family/caregiver feel comfortable;
- Share information about the individual’s goals, preferences, strengths and values with the individual’s entire care team;
- Use assessment approaches that take into account an individual’s entire history, its impact on his/her health, and support well-being and strengths (i.e., recovery-oriented and trauma-informed);
- Promote community integration, social supports, and care coordination, including opportunities for self-directed care to the greatest extent feasible; and
- Identify family/caregivers’ needs and the natural supports and home- and community based resources that enable them to provide assistance aligned with the individual’s needs and preferences, and ensure they get the training/support they require.
ATTRIBUTE 2: Each individual’s needs are addressed in a compassionate, meaningful, and person-focused way and incorporated into a care plan that is tailored, safe, and timely.
Delivery systems:
- Support the individual and his/her family/caregivers to guide the care plan to thegreatest extent feasible;
- Use a collaborative partnership approach to decision-making with the individual and his/her family/caregivers;
- Develop care plans that address daily living needs;
- Empower each individual with tools and strategies to promote his/her strengths and self-management of care within the care plan; and
- Use individual choice and priorities to help guide the most appropriate medical and social support strategy that is accessible and aligned with both the individual’s values and the family/caregivers’ needs.
ATTRIBUTE 3: Individuals have a cohesive, easily navigable delivery system so that they can get the services and information they want by themselves or with support when needed, and avoid the services they do not need or want.
Delivery systems:
- Ensure high-quality, coordinated, integrated, and accessible services that meet an individual’s full set of care needs (including, primary care, behavioral health care and substance use disorder treatment, LTSS, and technological assistance) in the most appropriate setting;
- Provide timely information on the benefits, costs, and risks of care and service options that individuals and their family/caregivers can understand and evaluate alongside their needs, values, and preferences in order to make decisions;
- Ensure that the individual is at the center of decision-making regarding care and services, and a full partner with their entire care team;
- Support timely, uninterrupted care and service delivery via an accountable primary point
of contact who understands the complete picture of the individual’s needs and has the authority and services and supports to connect the individual and family/caregivers to needs and services, as well as grievances and appeals processes across settings and systems; - Ensure that care teams effectively communicate with the individual, family/caregivers, and each other to support continuous, coordinated, and integrated care;
- Acknowledge that circumstances and environment affect individuals’ ability to navigate care and services, and tailor support to reflect these circumstances; and
- Provide culturally competent care and services tailored to each individual, as well as their family/caregiver, and the individual’s strengths, health literacy, language proficiency, and social/environmental circumstances.
ATTRIBUTE 4: Individuals and their family/caregivers continually inform the way the delivery system is structured to ensure that it is addressing their needs and providing resources tailored to them.
Delivery systems:
- Solicit and are responsive to ongoing collective input from individuals and the family/ caregivers served;
- Provide ways for individuals and their family/caregivers to raise issues outside of the delivery system’s formal grievance and appeal channels (i.e., hold regular local forums to solicit input);
- Support meaningful input by individuals and their family/caregivers for continuous improvement; and
- Evolve based on individuals’ and family/caregivers’ input into design, implementation, and evaluation to ensure the system is responsive to all individuals being served and their family/caregivers.
Key Definitions
The following two definitions were developed to guide the working group consensus process:
- Adults with complex care needs: Individuals having two or more mental and/or physical chronic conditions, and additional functional limitations that collectively have an effect on health status and quality of life.
- Essential Attribute: A feature regarded as a characteristic or inherent part of care delivery by providers serving adults with complex care needs, which affects its success or failure.
Below are definitions for terms used in Figure 1, which are drawn from existing sources:
- Behavioral health care: Refers to services that encompass prevention and promotion of emotional health; prevention of mental and substance use disorders, substance use, and related problems; treatments and services for mental and substance use disorders; and recovery support.2
- Community and social supports: Refers to services and supports that are not LTSS that promote independence, well-being, self-determination, social connectedness and community inclusion in meaningful, desired activities of individuals with complex care needs, supporting each individual to remain in his/her home and/or community.3 Community and social supports include items such as housing, transportation, employment, and education.
- Family/caregiver: Broadly defined, refers to any relative, partner, friend or neighbor, as well as paid caregivers, who has a significant personal relationship with, and who provides a broad range of assistance for an adult with complex care needs.4,5
- Long-term services and supports (LTSS): Refers to assistance with activities of daily living (ADLs) and instrumental activities of daily living (IADLs) provided in homes or community residences or in institutional settings to people with complex care needs who cannot perform these activities on their own due to a physical, cognitive, or chronic health condition that is expected to continue for an extended period of time, typically 90 days or more. LTSS also include supports provided to family members and other unpaid caregivers.6
- Primary/acute care: Primary care refers to care provided by physicians, nurse practitioners, physician assistants or other qualified health professionals specifically trained for and skilled in comprehensive first contact and continuing care for persons with any undiagnosed sign, symptom, or health concern. Primary care services include health promotion, disease prevention, health maintenance, counseling, patient education, diagnosis and treatment of acute and chronic illnesses.7 Acute care refers to a type of primary care that includes all promotive, preventive, curative, rehabilitative or palliative actions whose primary purpose is to improve health and whose effectiveness largely depends on time-sensitive and, frequently, rapid intervention.8
The following members of the working group affirm their support and commit to advancing the essential attributes produced through this consensus process.
G. Lawrence Atkins
Executive Director
Long Term Quality Alliance
Melanie Bella
Independent Consultant
Rich Bringewatt
Co-Founder and CEO
National Health Policy Group
Co-Founder and Chair
SNP Alliance
Helen Burstin
Chief Scientific Officer
National Quality Forum
Bruce Chernof
President and CEO
The SCAN Foundation
Jennifer Dexter
Assistant Vice President, Government Relations
Easterseals
Lynn Friss Feinberg
Senior Strategic Policy Advisor
AARP Public Policy Institute
Jennifer Goldberg
Directing Attorney
Justice in Aging
Ann Hwang
Director
Community Catalyst, Center for Consumer
Engagement in Health Innovation
Alice Lind
Manager
Grants and Program Development
Washington State Health Care Authority
Debra Lipson
Senior Fellow
Mathematica Policy Research
Margaret E. O’Kane
President
National Committee for Quality Assurance
Pam Parker
Medicare-Medicaid Integration Consultant
Minnesota Department of Human Services
Carol Regan
Senior Advisor
Community Catalyst, Center for Consumer
Engagement in Health Innovation
Those listed here are endorsing the Essential Attributes in their capacities as individual members of the working group.
Additional Working Group Members
The working group would also like to thank the following ex-officio members and additional participants for their time and thoughtful contributions to developing the Essential Attributes:
Gretchen Alkema
Vice President of Policy and Communications
The SCAN Foundation
Eliza Navarro Bangit
Director
Office of Policy Analysis and Development
Administration for Community Living
Department of Health and Human Services
Stephen Cha
Director
State Innovations Group
Centers for Medicare & Medicaid Services
Tim Engelhardt
Director
Medicare-Medicaid Coordination Office
Centers for Medicare & Medicaid Services
Marcus Escobedo
Senior Program Officer
The John A. Hartford Foundation
Stephanie Gibbs
Senior Program Officer
Center for Health Care Strategies, Inc.
Deidre Gifford
Director of State Policy and Programs
National Association of Medicaid Directors
Erin Giovanetti
Research Scientist, Performance Management
National Committee for Quality Assurance
Allison Hamblin
Vice President for Strategic Planning
Center for Health Care Strategies, Inc.
Susan Mende
Senior Program Officer
Robert Wood Johnson Foundation
MaryBeth Musumeci
Associate Director
Kaiser Commission on Medicaid and the
Uninsured
Wally Patawaran
Program Officer
The John A. Hartford Foundation
Lisa Patton
Director
Division of Evaluation, Analysis, and Quality
Center for Behavioral Health Statistics and
Quality
Substance Abuse and Mental Health
Services Administration
Kali Peterson
Program Officer
The SCAN Foundation
Diane Rowland
Executive Vice President
Kaiser Family Foundation
Executive Director
Kaiser Commission on Medicaid and the
Uninsured
René Seidel
Vice President of Programs and Operations
The SCAN Foundation
Nidhi Singh Shah
Health Policy Analyst
Center for Clinical Standards and Quality
Centers for Medicare & Medicaid Services
Emily Zyborowicz
Manager, Research and Identification
Peterson Center on Healthcare
Acknowledgements
The SCAN Foundation is grateful for the assistance of the Alliance for Health Reform and Health Management Associates. The Alliance for Health Reform is an independent not-for-profit organization that facilitated the working group process. Health Management Associates is an independent, national research and consulting firm in the health care industry that provided technical assistance and drafted the working group products.
Download the publication for all visuals and complete references.
Continue Reading
The SCAN Foundation aims to identify models of care that bridge medical care and supportive service systems in an effort to meet people’s needs, values, and preferences. Care coordination is a central component of this vision, which ultimately leads to more person-centered care. This brief outlines The SCAN Foundation’s vision for care coordination in a person-centered, organized system.
This policy brief describes California’s results in the 2014 Long-Term Services and Supports State Scorecard, identifying areas for improvement as well as policy opportunities to transform and improve the state’s system of care.
To succeed in this era of health system transformation, plans and providers bearing risk – in an accountable care organization (ACO) for example – will need strategies for managing a broad array of care needs for high-risk beneficiaries across multiple settings of care. Download this fact sheet to learn more.