California’s Use of Federal and State Policy Flexibilities to Ensure Access to Long-Term Services and Supports During the COVID-19 Pandemic
summary
This policy brief takes a closer look at how California has implemented federal flexibilities to ensure the state’s long-term services and supports (LTSS) system is responsive to the needs of older adults and people with disabilities during the COVID-19 pandemic.
Date Updated: 06/24/2020- california,
- complex care,
- coordinated care,
- COVID19,
- ltss,
- medicaid,
- medicare,
- person-centered care,
- The SCAN Foundation,
Introduction
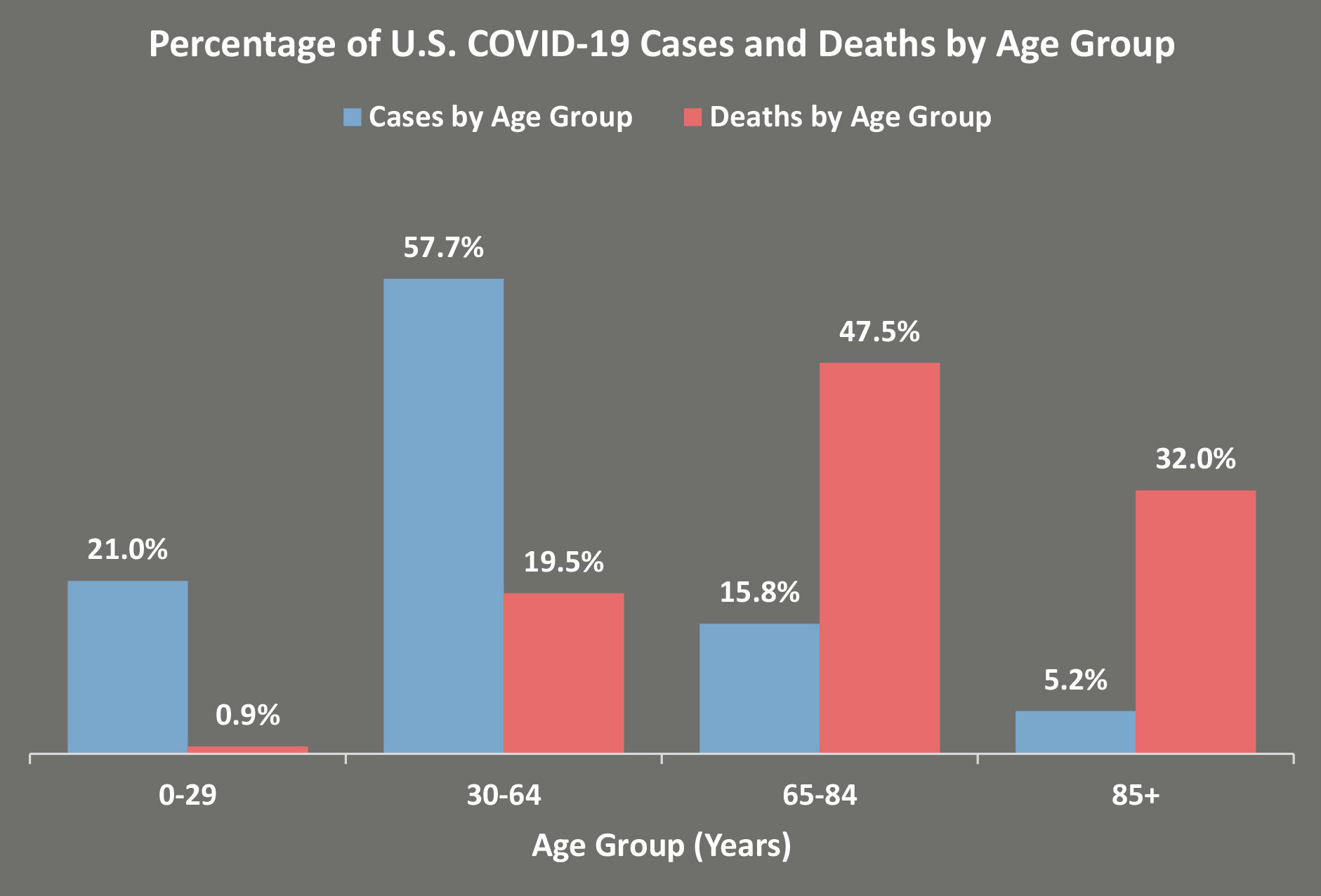
The emergence of the COVID-19 virus has fundamentally shaken the nation’s social, demographic, political, economic, and health care landscapes with two million cases and 115,644 deaths nationally as of June 15.1 Simultaneously, it has exposed underlying vulnerabilities in systems serving older adults, people with disabilities, and their family caregivers. Older adults have been disproportionately impacted with people age 65 and older representing 80 percent of COVID-19 related deaths, and people age 85 and older representing 32 percent of deaths.1 In addition, communities that have historically experienced inequities and health disparities have been more severely impacted by COVID-19. For example, Black Americans represent only 13 percent of the U.S. population, but make up 23 percent of COVID-19 related deaths.2 With the intersectionality of age, race, gender, and class, risk of severity builds.
California implemented stay-at-home orders in March following the recommendations by public health experts. This significantly impacted older adults and people with disabilities, especially those with high care needs. Social distancing restrictions and bans on visiting people in hospitals, nursing facilities, and assisted living facilities have compounded the impacts of isolation and loneliness experienced by older adults. Prior to COVID-19, 1 in 4 older Americans reported being isolated, and 40 percent reported being lonely. Since March, these numbers have tripled. Research has shown that social isolation substantially increases one’s risk of stroke, heart disease, depression, and dementia.2 Individuals who use long-term services and supports (LTSS) are particularly vulnerable to contracting COVID-19 and experiencing severe symptoms due to advanced age and/or living with one or more chronic conditions. Many of these same people are also at risk for nursing home placement. Without access to LTSS in the home and community, many older adults and people with chronic conditions could end up in institutional settings, which have been hardest hit with COVID-19 related deaths. Thus, it is in individuals’ and the state’s best interest to avoid the unnecessary institutionalization of this at-risk population. Federal response to the pandemic has allowed states to request flexibilities through the Centers for Medicare & Medicaid Services (CMS) in order to continue providing LTSS and mitigate risk. The time frame for the flexibilities depends on the Secretary of the U.S. Department of Health & Human Services’ public health emergency declaration which can last up to 90 days unless extended.3,4 In early June 2020, Manatt Health took a broad look across states and identified ways they have leveraged these new flexibilities to ensure access to LTSS.
California’s Response to LTSS Flexibilities
California’s LTSS system serves individuals both at home and/or in congregate settings (e.g., senior centers, adult day health centers, nursing facilities). For many LTSS programs, the mode of service delivery had to evolve in response to the public health directives. Home- and community-based services (HCBS) operating at congregate sites quickly adjusted to offer services remotely or at an individual’s home. Providers, in partnership with the state, developed alternatives to ensure people could access the support they needed at home while mitigating risk, putting precautions in place, and creating backup systems for providers. California utilized the flexibilities afforded by the federal government to ensure the state’s LTSS system responds to individuals’ evolving needs during the COVID-19 pandemic. At the policy level, tracking California’s implementation of flexibilities enables state leaders to consider how these modifications could shape services and supports in the future. The tables below identify regulatory flexibilities and administrative actions California has implemented that impact where and how LTSS is provided to meet individual care needs during this pandemic. Core themes include virtual care management, access to services, alternate care sites, provider capacity, and consumer protections. To consider flexibilities through a person centered lens, the table includes a statement on Impact on the Person, describing what the care experience might look like for the individual. Each table includes hyperlinks to the different programs and policy authorities. A glossary of acronyms is at the end of the document.
Virtual Care Management
These policy flexibilities and administrative actions seek to ensure individuals can access LTSS while minimizing their risk of exposure to COVID-19 by expanding the use of telehealth in place of in-person visits for care management activities.
| Impact on the Person | Program Flexibility or Action | Program | Authority |
| Individuals can be assessed for services and initiate care plans remotely to help them obtain the right supports when needed. | Allows assessments and other required face-to-face interactions for HCBS to be completed remotely (e.g., record review, telephone, video). | CCT | 1915 (c) Waiver Appendix K Amendment |
| HCBA | |||
| MSSP | |||
| HHS | 1135 Blanket Waiver | ||
| IHSS | 1135 Waiver | ||
| PACE | State Guidance | ||
| Allows physician services to be provided via telehealth. | Medi-Cal | 1135 Blanket Waiver | |
| Individuals will experience reduced risk to COVID-19 exposure with extended assessment time frames. | Extends reassessment period from once every 12 months to once every 18 months. | IHSS | 1135 Waiver |
| Extends assessment completion period from five to 30 days. | HHS | 1135 Blanket Waiver | |
| Extends assessment update period from 15 to 21 days. | Hospice | ||
| Individuals have a variety of options to complete required forms and approve care plans in order to prevent delays in getting services. | Forms requiring participant or legal representative’s signatures can be signed, scanned, and emailed to the CCA, or signed digitally. Signed hard copies should be saved until CCAs can retrieve them. | ALW | 1915 (c) Waiver Appendix K Amendment |
| Allows Medi-Cal-only providers to accept an individual’s verbal approval of care plan changes. | HCBS Waiver | 1135 Waiver |
Access to Services
These policy flexibilities and administrative actions seek to ensure individuals can access needed services and supports during the pandemic by providing services in new ways, removing prior authorization requirements, and easing administrative requirements.
| Impact on the Person | Program Flexibility or Action | Program | Authority |
| Individuals impacted by COVID-19 are allowed more time to meet enrollment and re-enrollment requirements in order to keep existing access to certain HCBS. | Suspends 60-day enrollment period for applicants unable to complete the application process and/or secure a bed in an assisted living facility due to COVID-19. Applicants can keep ALW slots through June 30, 2020, without being placed back on the wait list. | ALW | 1915 (c) Waiver Appendix K Amendments |
| Extends 31-60 day ALW re-enrollment period through June 30, 2020, for people who moved from an assisted living to a hospital/other care facility and cannot return due to COVID-19. | |||
| Extends the 30-day re-institutionalization disenrollment period through June 30, 2020, for any participant who must remain in an institutional setting beyond the 30-day limit because they, or their caregiver(s) have contracted the virus, and/or if it is unsafe for them to return to the community due to threat of exposure to the virus. | CCT | ||
| Pauses waiver disenrollment of people who are reinstitutionalized, beyond the 30-day limit, for those (or a caregiver) who are impacted by COVID-19. | HCBA | ||
| Individuals can find a backup attendant if the regular attendant is unavailable due to COVID-19 or caring for a family member. | Authorizes implementation of a backup provider system. | IHSS | All County Letter |
| Homeless individuals have additional support to locate temporary housing in order to minimize exposure to COVID-19. | Allows reimbursement for temporary, emergency housing. | WPC | 1115 Waiver |
| Individuals can access certain services more easily and efficiently. | Suspends prior authorization requirements. | Medi-Cal FFS | 1135 Waiver |
| Individuals have flexible transportation options to mitigate COVID-19 exposure. | Allows individuals to use safest available transportation for non-medical and non-emergency transportation. Medical necessity is not criteria for use and payment. | NMT/NEMT | State Guidance |
| Individuals continue to receive CCT services to transfer out of SNFs to the community. | Extends the Money Follows the Person program. | CCT | CARES Act |
| Individuals with Medicare can get medical equipment fixed or replaced more quickly. | DME Medicare Administrative Contractors can replace lost, damaged, unusable DME without meeting face-to-face, a new physician’s order, or new medical necessity documentation. | DME | 1135 Blanket Waiver |
| Individuals with Medicare can access needed skilled nursing services without getting a surprise hospital bill. | Waives Medicare’s three-day hospitalization requirement to cover SNF services. | SNF | 1135 Blanket Waiver |
| With reduced administrative requirements, staff can dedicate more time to providing care. | Waives 14-day time frame requirement for Minimum Data Set assessment and transmission. | SNF | 1135 Blanket Waiver |
Alternate Care Sites
These policy flexibilities and administrative actions seek to allow individuals access to HCBS while mitigating risk of exposure to COVID-19 by expanding the allowable settings where HCBS may be provided.
| Impact on the Person | Program Flexibility or Action | Program | Authority |
| Individuals can continue to have health and non-health needs met at home instead of site based care. | Allows home-delivered meals in place of congregate meals. | CBAS | All Center Letter |
| Allows physical and occupational therapies to be provided at home. | |||
| PACE participants who have to move out of the service area temporarily due to COVID-19 can continue to receive services. | PACE can continue to serve people who temporarily move out of the service area due to COVID-19. The change of address does not need to be reported to Medi-Cal. | PACE | CMS PACE Memo; State Guidance |
| PACE can place people in facilities outside the service area for the length of the COVID-19 crisis if there is a lack of available beds in the service area. | |||
| Individuals can have their IHSS hours adjusted to address services and supports no longer available due to COVID-19. | Counties can adjust authorized hours to compensate for HCBS no longer available due to COVID-19 (e.g., services at congregate sites). | IHSS | All County Letter |
| Individuals who need support beyond what a hospital provides can receive HCBS in the hospital. | Allows Medicaid HCBS (e.g., case management) to be provided in acute care hospitals when these services 1) meet needs not met through hospital services, 2) are not a substitute for services the hospital is obligated to provide, and 3) are designed to ensure smooth transitions between acute care and home- and community-based settings. | HCBS | CARES Act |
Provider Capacity
These policy flexibilities and administrative actions seek to expand the pool of LTSS and medical providers and workers to ensure individuals can receive services to which they are entitled during the COVID-19 pandemic.
| Impact on the Person | Program Flexibility or Action | Program | Authority |
| Individuals may experience less disruption in care and access care when needed with a broader workforce working at the top of their professional license. | Allows nurse practitioners to provide care to the fullest extent possible depending on state regulations. | FQHC/RHC | 1135 Blanket Waiver |
| Waives requirement that Medicare patients be under the care of a physician, so hospitals can use other practitioners to the fullest extent possible (dependent on state regulations). | Medicare | ||
| Allows physicians to delegate any tasks to a physician assistant, nurse practitioner, or clinical nurse specialist depending on state regulations. | NF | ||
| Gives California departments of Public Health and Consumer Affairs authority to amend scopes of practice. | Executive Order | ||
| Waives restrictions on the number of nurse practitioners that can be supervised by a physician. | California Department of Consumer Affairs Waiver | ||
| Waives supervision requirements for physician assistance. | |||
| Individuals have more options to have their needs met. | Permits payment for services rendered by family caregivers or legally responsible individuals. | HCBA | 1915 (c) Waiver Appendix K Amendment |
| Permits unlicensed waiver personal care services providers as long as they are currently IHSS providers. | |||
| Allows CNAs to provide Private Duty Nursing, in addition to currently authorized HCBS Waiver nurse providers (i.e., RN, LVN, and CHHA) and home health agencies. | |||
| Individuals will be able to access therapy services quicker with minimal disruption. | Allows OT to perform the initial and comprehensive assessment for all patients receiving therapy services, to the extent permitted under state law, regardless of whether OT is the service that establishes eligibility. | HHS | 1135 Blanket Waiver |
Consumer Protections
These policy flexibilities and administrative actions seek to ensure an individual’s safety and access to services by ensuring continued access to the LTC Ombudsman and adjustments to fair hearing timelines.
| Impact on the Person | Program Flexibility or Action | Program | Authority |
| Makes the fair hearing process more responsive to individuals’ needs during the COVID-19 crisis. | Modifies the amount of time health plans have to resolve an appeal to no less than one day before a fair hearing can be requested. | Medi-Cal Managed Care | 1135 Waiver |
| Provides Medi-Cal enrollees an additional 120 days to request a fair hearing. | Medi-Cal FFS /Medi-Cal Managed Care | ||
| Individuals still have access to the LTC Ombudsman even though site visits are restricted. | Allows LTC Ombudsman to have direct virtual access to residents in LTC facilities. | LTC Ombudsman | CARES Act |
Conclusion
The COVID-19 crisis created opportunities for new building blocks of care oriented toward the person-centered experience and outcomes. Learning from the COVID-19 flexibilities, policymakers and providers can consider how these flexibilities might be applied in the future—post COVID-19. To help set a course for permanent LTSS systems change, the flexibilities should be evaluated in relation to California’s Master Plan for Aging goals developed by the Stakeholder Advisory Committee. Additionally, evaluation of the flexibilities alongside person-centered criteria would serve to identify those that have been most impactful in improving care. Such information could help California determine which flexibilities should remain, be modified, or be removed when the COVID-19 crisis has passed.
Glossary of Acronyms
Download the publication for all visuals and complete references.
Continue Reading
The California Medicaid Research Institute (CAMRI) developed an integrated and longitudinal database containing Medi-Cal and Medicare claims and assessment data of LTSS recipients in California in 2008. CAMRI’s integrated database provides a unique opportunity to look at characteristics and program spending across the entire care continuum for beneficiaries with LTSS needs within Medi-Cal and for dual eligibles across Medicare and Medi-Cal. This report focuses on LTSS use and spending in the eight duals demonstration counties.
In this paper, the National Committee for Quality Assurance (NCQA) discusses prior integration efforts; introduces a model for integrated entities and a framework for assessing and promoting quality of integrated care; and explores the challenges to implementing and achieving the goals of person-centered, integrated care for Medicare-Medicaid beneficiaries. They use the word “framework” to describe the key concepts underlying the structure and process measures; it can also be expanded to include the content of performance measures as companions to the structure and process measures.
Following on previous reports describing the population who uses Medi-Cal-funded long-term services and supports, the California Medicaid Research Institute has produced a report that describes key characteristics of the population using LTSS across each of the state’s 58 counties. This report describes spending and service use patterns across the 58 counties.